New drug target for schizophrenia
Researchers in Japan have identified lower levels of a crucial lipid in the brains of folks with schizophrenia, which could lead to new treatments for the mind disorder.
Schizophrenia is a mental illness that can profoundly change an individual’s perception of reality. Around 2.4 million adults in the United States live with schizophrenia, that may cause symptoms such as for example hearing voices, struggling to arrange thoughts, and having visual hallucinations and delusions.
Although society is starting to discuss mental health more openly, because of initiatives such as for example Mental Health Month, there continues to be a lot of stigma around schizophrenia.
Living with schizophrenia can also be extremely challenging. Treatment plans are limited, and antipsychotics, which will be the standard first-line treatment, are ineffective in lots of patients.
Antipsychotic drugs may also have unpleasant unwanted effects, including considerable weight gain, tiredness, and restless muscles. One study even linked first generation antipsychotic drugs to the increased loss of brain tissue in people with schizophrenia.
However, a fresh study from the RIKEN Center for Brain Science (CBS) in Japan could start a different avenue for drug development - the one that relates to changes in lipid metabolism.
White matter deficits
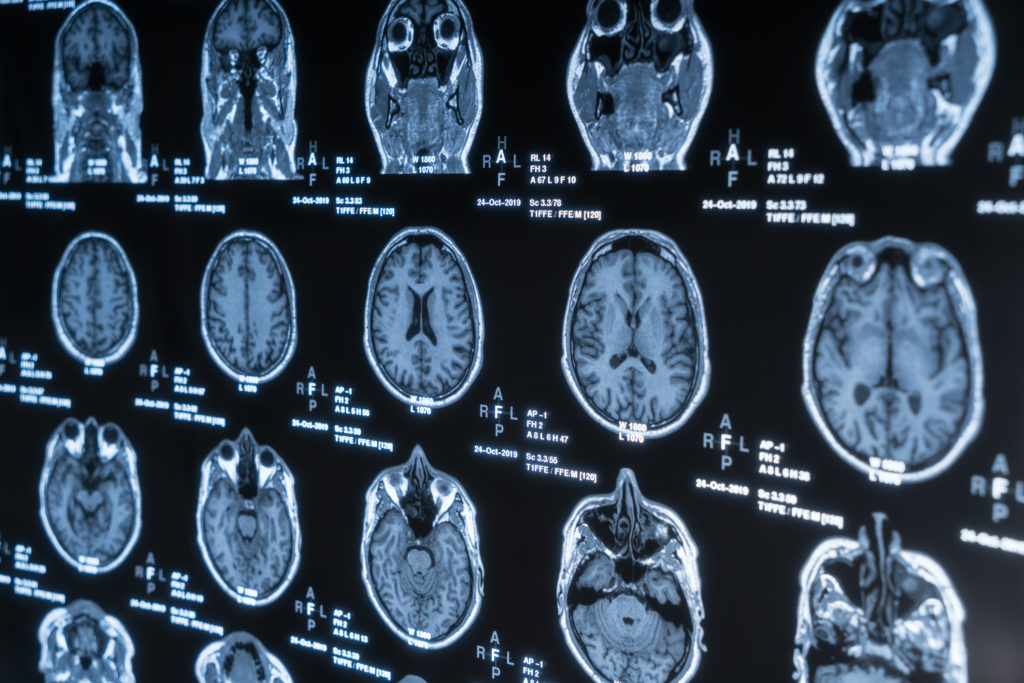
The study targets white matter, the area of the brain comprising axons that carry nerve impulses between neurons. Research has identified a reduction in white matter in persons with schizophrenia.
White matter gets its name from its light color, which is because of the lipid-dense myelin sheaths that surround axons, facilitating the rapid conduction of nerve impulses. Loss of myelin is associated with numerous neurological conditions, most notably multiple sclerosis.
Fatty molecules called sphingolipids are essential in the forming of myelin, and previous studies have shown differences in the levels of these molecules in persons with schizophrenia. However, many questions remain unanswered.
To look at the connection between sphingolipids and schizophrenia in more detail, the researchers behind the new study analyzed the degrees of these molecules in the postmortem brain tissue of 15 persons with schizophrenia. They carried out the same analysis on the same number of age- and sex-matched controls.
An interdisciplinary approach
The researchers used mass spectrometry, a method typically more familiar to chemists. This technique identifies the particles present in a sample by measuring their mass, which it can by bombarding the sample with electrons.
“This was the first psychiatric study of the postmortem brain to use mass spectroscopic analysis, and our discovery wouldn't normally have already been possible without our newly established comprehensive way of screening sphingolipids,” explains Dr. Takeo Yoshikawa, team leader at RIKEN CBS.
The team discovered that degrees of a sphingolipid called S1P were low in persons with schizophrenia than in those without this problem. Levels were lower in a region of the brain called the corpus callosum - the greatest collection of white matter in the mind, which connects its two hemispheres. Abnormalities in this area could cause irregular communication between neurons.
To determine whether this mechanism is common across mental disorders, the scientists also analyzed the brains of folks with bipolar disorder and major depressive disorder.
They discovered that S1P levels in these persons were normal, indicating that the deficiency is specific to schizophrenia.
A new treatment?
Further experiments suggested that the challenge may be due never to an impaired production of S1P but to the abnormal degradation of the lipid.
If this is actually the case, designing drugs to avoid the break down of S1P could help treat schizophrenia. The team hopes that finding can help reinvigorate drug development for the problem.
“Because we don’t have another angle on what causes schizophrenia, many pharmaceutical companies are pulling out of schizophrenia-related drug development. Hopefully, our findings can offer the brand new angle with a fresh target for drug development.”
- Dr. Takeo Yoshikawa
The researchers say that it's possible that the prevailing multiple sclerosis treatment fingolimod (Gilenya) - which targets the S1P receptor - could be effective, eliminating the need for an extended drug development process.
However, it remains unclear whether Gilenya works as cure for schizophrenia, and more research is necessary to understand the specific role that S1P plays in the problem. The initial step is to begin focus on animals, Yoshikawa says.
Source: www.medicalnewstoday.com
