As doctors go virtual, pandemic turbocharges telemedicine
Will visiting the doctor ever be the same again?
In just a matter of weeks, the coronavirus pandemic sparked a technological revolution in healthcare systems around the world that might otherwise took years.
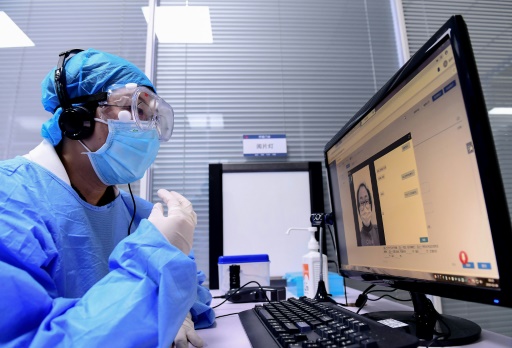
Spurred on simply by fears of contagion in wards and waiting around rooms, many doctors are exchanging the face-to-face meetings which have always underpinned standard practice, with patient consultations by phone and online video software.
One of the most radical alterations have been around in principal healthcare, where doctors possess often faced shortages of protective products, but specialists in from mental well being to eye care have also turned to technology to take care of patients far away.
"General practice possesses undergone significant changes in the manner GPs and our clubs have delivered patient attention through the pandemic -- and the acceleration in which these changes were applied has been remarkable," Professor Martin Marshall, Chair of Britain's Royal College of GPs told AFP.
As the virus pass on, health authorities in the UK, Europe and somewhere else updated guidance on from data coverage to developing trust remotely.
AMERICA rolled back restrictions on access to telemedicine, and eased privacy regulations to permit people to use platforms like Skype and FaceTime.
"People are now seeing this model, which we thought would take a long time to develop. And it's almost certainly been accelerated by ten years," Chris Jennings, US insurance policy consultant and former Light House health care adviser advised STAT news recently.
Globally, 58 percent of surveyed countries are now using telemedicine, the Environment Health Group said Monday, adding the figure was 42 percent among low income nations.
Layla McCay, a director at the NHS Confederation representing British health care companies, told AFP that almost all of the UK's 1.2 million daily face-to-face principal caution consultations were done remotely "in the space of weeks".
But there have been challenges.
"My first video discussion was chaos. Builders had been drilling, the microphone failed, a colleague walked in, and lockdown was imminent," Camille Gajria, a health care provider and clinical coaching fellow at Imperial College London, told the British Medical Journal.
She said teleconsultations could be efficient but warned of "cognitive bias" -- a doctor, for instance, might assume a child playing in the backdrop may be the one being discussed.
Additionally, there are concerns that vulnerable patients will dsicover it difficult to speak about mistreatment in the home, while elderly persons could battle to navigate unfamiliar technology.
Telemedicine may seem just like a merchandise of the web age, but it has been around for many years, developing alongside interaction technology.
One big leap came during the space race of the 1960s, when scientists concerned about the result of zero gravity on the human body. Would it not impede bloodstream circulation or breathing?
To find out, both US and Soviet Union conducted evaluation flights with animals installed to medical monitoring devices that transmitted biometric data back to scientists on the planet. Later, longer missions intended astronauts needed devices that could diagnose and support treat medical emergencies.
NASA went on to build up terrestrial telemedicine, including a good project to provide healthcare to the isolated Tohono O'odham reservation found in Arizona, along with disaster response found in the 1985 Mexico City and 1988 Armenia earthquakes.
As the coronavirus pandemic has driven sweeping changes in the manner many people see their local doctor, it has additionally highlighted the purpose telemedicine can take up in connecting clinicians with distant communities.
In India, which includes just 8.6 medical employees per 10,000 persons according to 2018 WHO figures, the majority of doctors are concentrated in urban centres, although some 70 percent of people are in rural areas.
Ayush Mishra, founder of the telehealth company Tattvan, said this implies persons outside bigger towns are often forced to seek medical tips from overstretched or perhaps ill-qualified practitioners.
His business, among an increasing number of telehealth providers in India, operates 18 clinics, mostly ATM-style booths that are manned by a medical assistant who can take vital measurements and associated with doctors in hostipal wards in larger towns.
The firm languished in a legal grey zone for a long time before coronavirus crisis spurred the federal government into broadening regulatory approval for virtual consultations. Right now he hopes to available a huge selection of clinics around the united states.
Mishra traces his enthusiasm for telemedicine to a good horrific motorbike accident when he was a biomedical engineering student in the northern metropolis of Jaipur.
Severely injured, he was driven ten hours to his hometown in Uttar Pradesh, before falling right into a coma mainly because a local doctor performed surgery.
His friends and family was overwhelmed by "panic" until his father spoke by phone to a surgeon at a medical center in Delhi, enabling them to set up treatment in the city.
Mishra lost his leg, but told AFP the experience inspired him to want to equalise medical gain access to for individuals in smaller towns.
"You have to be in a position to offer this access -- it's a human right," he said.
Internet-connected thermometers, pulse oximeters to measure oxygen levels, and smart gadgets that monitor essential signs are widening the scope of what is possible in remote drugs.
Within an April article for JAMA Neurology, specialists from the Netherlands and U.S. explained telemedicine is actually a useful application for in-home training, such as activities for survivors of stroke. Patients, they noted, could be monitored via sensors in wristwatches or phones.
"We hope that this current COVID-19 crisis will be resolved. However, it really is as the older saying runs: 'never waste an excellent crisis'," they said.
"Telemedicine for chronic neurological disorders should become section of the new normal instead of the exception."
Marshall said there are still many routine procedures -- vaccinations, blood checks and physical examinations -- that cannot be done remotely.
"Those coping with multiple circumstances and other complex overall health needs really benefit from seeing their doctor in person -- and this is helpful for the GP, aswell," he said.
But he added that study supports the consumption of remote consultations for clients with simple circumstances, or who've "transactional" needs such as a repeat prescription.
Many say they need at least a few of the changes to stay.
"It possesses certainly turbocharged the digital transition nationally," said McCay of the NHS Confederation.
"Plenty of feedback from our users shows the culture has got fundamentally changed, and clinicians who had been perhaps previously resistant to digitisation are actually realising its benefits."
"We can't head out backwards," she added.
